The human body is a complex system that responds differently when invaded by a virus or disease. Why can only males donate bone marrow and can females donate bone marrow are the most concerned questions. To understand these questions properly, there is need to debate on them one by one. Thanks to science, which has provided us with numerous solutions and treatments to prevent chronic and deadly diseases. The stem cell donation process is one of the most effective and reliable procedures that can change the course of a patient’s life, particularly for those suffering from a life-threatening disease. Compared to females, males are the primary donors of bone marrow, and the transplant success rates are higher than those of female donors in the registry.
Therefore, we will discuss everything about bone marrow donation, including how it works, who can donate bone marrow, and more.
Let’s begin with the basics and understand the entire process and its significance.
What is Bone Marrow Donation?
It is a medical procedure in which healthy stem cells are collected from a donor to replace damaged or diseased bone marrow in a recipient. Basically, bone marrow is the soft, spongy tissue found inside bones that produces blood cells, including red blood cells, white blood cells, and platelets. The primary goal of the transplant is to restore the body’s ability to produce healthy blood cells and strengthen the immune system.
The bone marrow registry is one selfless act in which every person has the opportunity to make a significant difference in the lives of patients battling life-threatening diseases, such as leukemia, lymphoma, and other blood disorders. Contrary to popular belief, both males and females can donate bone marrow; however, there are specific reasons why males are preferred in some cases, although most donors are female.
Requirements for Donation:
But before you’re able to donate bone marrow, you first need to see if you meet the eligibility criteria. If you fulfill the bone marrow donation requirements, then you will be eligible for the final procedure.
These requirements are as following:
1. Age Limit:
The age of the donors should typically be between 18 and 60 years old. The ideal and more preferred age is 30 because younger stem cells tend to be healthier and more effective.
2. Good Health:
Donors must be in overall good health, without chronic medical conditions such as heart disease, diabetes, or autoimmune disorders. It is essential to have no-cancer history.
3. HLA Compatibility:
A Human Leukocyte Antigen (HLA) test is conducted to find the best possible genetic match between donor and recipient.
4. Free from Infections:
The donor must not have infectious diseases like HIV, hepatitis B or C, or other blood-borne illnesses.
5. Healthy Weight:
To make a safe transplant process, the donor should have a normal body mass index (BMI).
6. No Drug or Alcohol Dependency:
For efficient recovery, the donor must not have any substance abuse issues that could interfere with the procedure.
7. Non-Pregnant:
Pregnant women are not eligible to donate bone marrow.
8. Medical Evaluation:
A full medical examination and blood testing are required before donation to confirm suitability.
Moreover, the donors must be mentally and emotionally prepared, fully understanding the process and providing voluntary consent. Is bone marrow donation safe? Answer is meeting these requirements helps ensure that bone marrow donation is a safe and successful procedure, offering patients a renewed chance at life.
Understanding Bone Marrow and Its Role in Transplantation:
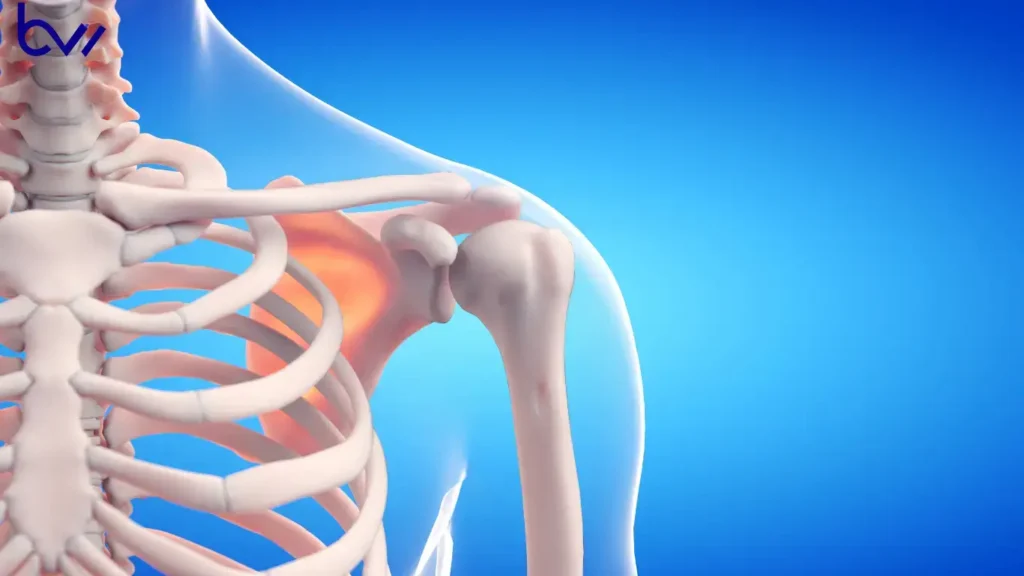
It is essential to comprehend the motivation behind bone marrow donation and how the immune response in transplantation can make a significant difference. To understand donor preferences, you have to know what bone marrow actually does. Essentially, it’s a soft, spongy tissue located inside the bones, primarily found in the ribs, hips, and sternum. According to science, it’s a factory for blood-forming stem cells that causes the production of:
- Red blood cells, which carry oxygen throughout the body.
- White blood cells, which fight infections.
- Platelets play a crucial role in blood clotting and wound healing.
The patients with severe immune disorders, such as:
- Leukemia
- Lymphoma
- aplastic anemia or certain genetic conditions
Their bone marrow stops functioning correctly. In such cases, doctors perform a bone marrow transplant (BMT), also known as a stem cell donation process. It will replace the destroyed and damaged marrow with new or healthy stem cells.
Who Can Donate Bone Marrow?
Specifically, regarding bone marrow donor eligibility, any healthy adult aged 18 to 55 can register as a donor. For general medical criteria for donors, they must have the following:
- Must be in good general health.
- Zero cancer history, severe infection, or heart disease
- Not have any transmissible diseases such as hepatitis or HIV
Can females donate bone marrow? People often ask this question. The answer is straightforward: anyone who meets the general donor criteria is eligible to donate bone marrow. The selection of a donor is not limited to gender, but other important factors can also influence the final decision.
HLA Matching — The Core of Bone Marrow Transplants:
In the selection of male vs female bone marrow donors, the process doesn’t stop at eligibility. A unique test called HLA typing (Human Leukocyte Antigen matching) is required, in which the donor is critically selected based on their specific high tissue compatibility.
These tissues are the proteins found on the surface of most cells in the body. They help the immune system distinguish between cells that belong to the body and those that do not. Therefore, the donor must match closely with the patient’s HLA as the patient’s body requires it in immense quantities. The patient’s immune system will reject the donated cells. In response, the body may react in worse ways and become attached, leading to Graft-versus-Host Disease (GvHD), a potentially severe condition.
Females produce HLA antibodies, and pregnancy can affect them, so it’s better to find a female donor who shares a close number of HLA types.
Why Are Male Donors Preferred?
When discussing donor selection guidelines, it is essential to highlight the critical aspect of selecting male donors—especially young males, such as those in their 30s, who are the major contributors to bone marrow registries. We will conduct a comparison that will elaborate on the prospects of male and female donors. The following points will help you to understand why male donors are preferred. These reasons are rooted in immunology, pregnancy history, stem cell yield, and transplant outcomes. Let’s explore them one by one:
1. Lower Risk of Graft-versus-Host Disease (GvHD):
The typical condition occurs when the patient’s immune system recognizes the recipient’s cells as a threat or finds them as foreign tissues. Medically, it’s a hazardous condition, and the consequences include:
- Organ damage
- Infections and even death
In male donors, the incidence of GvHD is lower; therefore, transplant success rates are higher compared to those in women. During pregnancy, the female body produces pregnancy-related antibodies, which are the leading cause of a higher number of GvHD encounters.
2. Higher Stem Cell Yield in Males:
Males and females exhibit differences in stem cell yield, which are attributed to their distinct body structures and masses. Men typically have larger frames and bodies; women, in comparison, tend to have smaller frames and bodies. Males are preferable for the following reasons:
- They produce a significant number of blood-forming stem cells.
- Either the collection process, starting from bone marrow harvest or peripheral blood stem cell collection, tends to yield more stem cells per session.
The success rate of bone marrow transplant depends on the settlement of donated cells in the recipient’s body. Young and healthy male donors provide the ideal cell quantity and quality needed for a successful transplant.
3. Fewer Medical Deferrals and Restrictions:
Another reason is the compatibility of male donors and their availability. If we compare this condition with females, they may be dealt with temporary restrictions, for example:
- Pregnancy or breastfeeding, during which donation isn’t allowed.
- Iron deficiency or anemia is more common in females.
Although pregnant females can donate later, it may prevent or slow down the donation process. However, male candidates can complete the process at any time by calling to donate.
4. Lower Levels of Alloimmunization:
This medical term refers to the process by which a person’s immune system produces antibodies in response to exposure to foreign antigens. An example of this is during blood transfusions, pregnancy, and after previous transplants. In the female body, they experience alloimmunization more especially during the pregnancy period.
So males never carry such antibodies, which makes them suitable and preferable stem cell donors for a registry.
Better Overall Transplant Outcomes:
According to bone marrow registry data and clinical research, the consistent trends are seen:
- Fewer complications are experienced in the recipients of male donors
- Higher long-term survival rates are found in patients who receive bone marrow from a young male donor.
Moreover, the pattern of GvHD was also found to be less in patients who have male donors. However, these are statistical measurements, but not absolute rules. In the medical world, where even a small action can make a significant difference, outcomes play a crucial role.
Does This Mean Women Cannot Donate? Absolutely Not!
Can females donate bone marrow? It is one of the most frequently asked questions whenever someone collects information about a bone marrow transplant. When we discuss bone marrow donation myths, one of them is that people think females can’t do it. Fortunately, women can donate bone marrow successfully. In fact:
- They are sharing a large portion of the bone marrow registry
- With blood stem cell donation, they performed life-saving transplants.
- Women have the best and closest HLA-matched bone marrow, indicating their greater compatibility and potential for undergoing the procedure.
According to statistics, females account for approximately 40% of donations worldwide. Especially nulliparous women who have never been pregnant are the ideal choice for bone marrow transplant because their bodies have not produced pregnancy-related antibodies. In short, males and females are equally competitive for donation.
Ethical and Medical Balance:
In the discussion of male versus female bone marrow donors, it is essential to understand that the criteria for transplant depend solely on medical outcomes and proven scientific evidence. It’s not about gender, but the best choice of survival for the patient.
Ethical principles and medical support are provided to both genders, encouraging them to join the match donor program. It is essential to encourage young people to participate in this race because every individual can save a remarkable life.
The Ideal Bone Marrow Donor Profile
If we shortlist the ideal donor characteristics, most transplant specialists will agree with the following table:
While every patient’s case is different, most transplant specialists concur that the **ideal donor** typically has the following traits:
| Characteristic | Preferred Type |
| Gender | Male |
| Age Range | 18–30 years |
| Pregnancy history | None |
| Health Status | Excellent, non-smoker, no chronic illness |
| Weight/BMI | Healthy range for optimal stem cell yield |
| Ethnic Background | Diverse (to improve registry representation) |
Note: The above table describes only the preferred choice, but not the rules. If a woman over 30 has the best HLA-matched bone marrow, then she will be the ideal candidate for a transplant.
What Happens During Bone Marrow Donation?
Is bone marrow donation painful? In many queries, people are often concerned about it. To understand this, we will elaborate on two methods of collecting stem cells. We ensure that after knowing them, it will eliminate all the fear and myths, so let’s have a look:
1. Peripheral Blood Stem Cell (PBSC) Donation:
It can be divided into three parts, in which:
- The donor is given medication for several days to increase stem cell production.
- Blood is drawn from one arm, stem cells are separated, and the rest of the blood is returned through the other arm.
- The process takes 4–6 hours and is a non-surgical procedure.
2. Bone Marrow Harvest:
The second method is also categorized into three parts, including:
- A surgical procedure performed under anesthesia.
- Doctors collect marrow directly from the pelvic bone using a needle.
- The body naturally replaces the removed marrow within a few weeks.
Is bone marrow donation safe? The answer is yes, in fact, both methods are safe and recommended. Only a few commonly found Side effects of donating bone marrow can be seen, including:
- Fatigue
- Soreness
- temporary bone pain, etc
Although the entire process is voluntary, all the donors are carefully monitored by medical professionals.
Global Statistics and Trends:
In recent years, due to awareness among people, they are now understanding the importance of the impact of bone marrow transplant. The global trends and statistics can underline the reality.
- The total number of bone marrow transplants yearly is around 50,000
- 70% of them rely on unrelated donors.
- The ratio of male donors is 60–70% and female donors still contribute about 40% of all life-saving procedures.
- The best outcomes statistically are achieved by young male donors under 30.
The statistics show that
Encouraging Everyone to Become a Donor
Can a stranger be a bone marrow match? If you have read this blog thoroughly, then you should know the answer. It’s not about any gender but the passion to serve humanity. Anyone can register with the simple registration process:
- Visit the website of the bone marrow registry.
- Provide the necessary health-related details to fill out the form
- For HLA typing, provide a saliva sample or a cheek swab.
Now, you have to wait for the patient who matched your HLA stem cell criteria. Whenever the clinic finds a patient, they will contact you for further medical tests and examination. If the registry determines you are a compatible match after all the tests, you will be able to save the lives of patients with leukemia, lymphoma, or other life-threatening diseases.
Conclusion:
So, why can only males donate bone marrow? It’s not true because females are equally capable of donating. Due to their availability and health traits, males are more preferred than females. Although there are no hard and fast rules, scientific evidence and medical outcomes suggest that males can undergo bone marrow transplants more frequently. They have a low risk of immune complications, high stem cell counts, and more consistent availability. Pregnancy is the main factors that eliminate the eligibility of female donors. By understanding the science behind donor selection and spreading awareness, we can all help save more lives through bone marrow donation.
FAQs:
Why can’t females donate blood?
Females often can’t donate blood temporarily due to low hemoglobin levels, pregnancy, or menstruation.
Who can be a 100% bone marrow match?
Usually, it comes from an identical twin or a perfectly matched sibling.
Can a daughter donate bone marrow to her father?
Yes, a daughter or even a family member can donate bone marrow to their family members. The only requirement is their genetic match.
Who cannot donate bone marrow?
Individuals with serious illnesses, infections, or autoimmune diseases are typically ineligible to donate bone marrow.